Four in five new heroin users started out misusing prescription painkillers, according to the American Society of Addiction and Medicine (ASAM).
“There’s a great deal of misinformation out there, and doctors strive to make their patients satisfied and to help patients feel they have some control over their illness,” said ASAM’s immediate past president Stuart Gitlow. “They give them what they are asking for, but opiates, really, are not your friend if you’ve got any form of chronic pain.”
Gitlow added that opiate-based medicine does not have value for people struggling with chronic pain.
Roughly 21.5 million Americans 12 or older had a substance use disorder in 2014, of which 1.9 million had a substance use disorder involving prescription pain relievers. “Opioid addiction is driving this epidemic, with 18,893 overdose deaths related to prescription pain relievers, and 10,574 overdose deaths related to heroin in 2014,” ASAM stated.
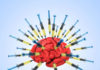
One key reason addiction to opioid painkillers is on the rise is because they’re being overprescribed by physicians. In 2012 alone, physicians approved 259 million opioid prescriptions, enough for every adult in the U.S. to have a bottle of pills.
Last March, the Center for Disease Control and Prevention (CDC) released a guideline with important information for primary care physicians prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. The guideline, now more relevant than ever, focused on when to initiate opioid prescriptions, and assessing, and addressing risks and harms. It also covered opioid selection, dosage, duration, follow-up and discontinuation.
Physicians are encouraged to better understand who qualifies for opioid prescriptions, but communities should also understand the risks involved when accepting to use these drugs.
“The public at large and people with pain would benefit from a better understanding of pain and its treatment in order to encourage timely care, improve medical management, and combat stigmatization,” a report released last March by the National Institutes of Health and the Institute of Medicine stated.
A checklist for physicians
The CDC provides a checklist for physicians prescribing opioids for chronic pain and recommends several careful considerations before writing a prescription, including:
- Setting realistic goals during pain and functions based on diagnoses, such as walking around the block.
- Checking that non-opioid therapies have been tried and optimized.
- Discussing benefits and evaluating risks such as addiction and overdose. Reviewing data from the prescription drug monitoring program (PDMP) is also recommended.
- Setting criteria for halting or continuing prescription opioids.
- Assessing baseline pain and functions by using the PEG scale (pain measured from zero to 10).
- Scheduling a reassessment within one to four weeks.
- Prescribing short-acting opioids that use the lowest dosage.
If a primary care physician is renewing a prescription without a patient visit, a return visit should be scheduled about three months from the last visit. When reassessing a return visit, a physician should only continue prescribing opioids after… (continue reading)